
The world is facing an unprecedented, growing problem with food allergens – but analytical scientists can help.
Research has revealed increasing rates of hospital admissions or hospital visits due to anaphylaxis in the US, Europe, Australasia and Asia, with 72% more children admitted to English hospitals in 2019 than just six years earlier. According to the BBC, data from multiple peer-reviewed sources also suggests that the rate of food allergies increased from around three per cent of the global population to around seven per cent between 1960 and 2018. Some 32 million Americans and up to 26 million Europeans are now thought to have food allergies, and the range of foods that people are sensitive to has also increased dramatically compared to decades ago. “(F)ood allergies have risen (…that) is unquestionably the case, to an absolutely crazy extent,” says emeritus professor of medical microbiology Graham Rook.
The increasing regulatory response
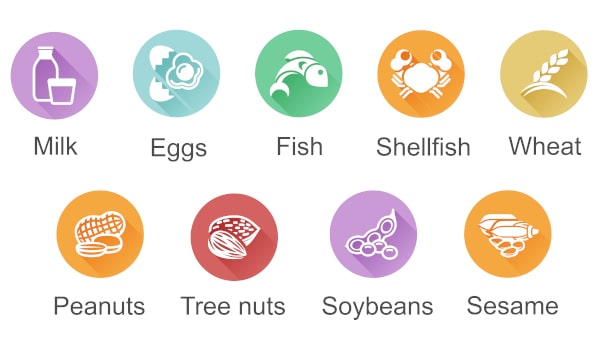
Trends such as these – and the absence of a conclusive answer to the question: ‘Why are food allergy rates rising?’ - have prompted governments to try and contain the problem by increasing regulation around the identification and labelling of food allergens. In 2004, the US Food Allergen Labeling and Consumer Protection Act (FALCPA) identified eight major allergens and mandated that foods or ingredients containing them must be specifically labelled. In the European Union, Regulation (EU) No 1169/2011 was implemented between 2014 and 2016, requiring that all pre-packaged foods display nutrition information. Moreover, foods containing any of 14 allergens that need to be declared by EU law must be included and emphasised in the list of ingredients. Last year, in response to the death from anaphylaxis of the teenager Natasha Ednan-Laperouse, the UK government further tightened up allergen labelling regulations by “requiring food businesses to include full ingredients labelling on pre-packed for direct sale (PPDS) foods.” President Joe Biden also approved the Food Allergy Safety, Treatment, Education, and Research (FASTER) Act in May last year, making sesame the ninth major allergen that US companies must display on food packaging from January 1, 2023.
The challenges and risks involved in identifying allergens
The food we eat can become contaminated with allergens in many ways, but happens broadly through two main avenues: undeclared allergens and cross-contamination. If any player in the production process – for example, a third-party supplier or repackaging company – should fail to label products properly, the consequences can potentially be serious or even fatal. Cross contamination is also a real danger if products are prepared in the same place as food allergens, if cleaning is inadequate, or when goods are stored close to allergenic materials. Allergen testing in laboratories is therefore a crucial line of defence for consumer safety and overall public health.
Food companies should also be conscious of the financial impact that allergen contamination can have on their profitability. Withdrawing products from sale due to undeclared allergens remains common and may account for around a third of all recalls. Moreover, more than one in four recalls costs companies between $10 million and $29 million without even accounting for damage to brand reputation. The former deputy commissioner for foods and veterinary medicine at the US Food and Drug Administration, Dr Stephen Ostroff, also calculated that the food industry could save at least $5 billion a year were it able to cut recalls by 50 per cent. Given the risks, regulations and potential rewards associated with food allergens, it is clearly vital to have confidence in the composition and labelling of our products, and laboratory analytical scientists can play a key role in ensuring this.
New foods + drinks = more regulation for allergens?
The boom in the development and sales of new foods - such as plant-based milk and meat substitutes - could also lead to more complex and stringent allergen labelling regulations in years to come. Many novel food products, such as legume-based meat alternatives, contain the same or similar proteins as are present in allergens. Meanwhile, another important future market – the development of synthetic cow’s milk based on artificially replicating milk- and whey proteins – poses potential regulatory issues around food labelling, because while the synthetic proteins are identical to those in dairy milk, they are not of animal origin. Therefore, regulations currently mandating that “cows’ milk” is identified in food items may need to be overhauled in order to take account of individual proteins, rather than detailing ingredients that may contain a variety of them. Clinical studies on allergy sufferers could also be necessary in order to determine appropriate testing guidelines for new foods – thus ensuring that all allergenic proteins of interest are detailed on product labels.

LGC adds over 70 InBio products to create unique new Dr Ehrenstorfer allergens range
LGC has teamed up with InBio, the leading manufacturer of purified allergen materials, to offer you a unique range of food allergen reference materials and ELISA 2.0 testing kits.
The addition of 74 InBio products to our already extensive portfolio means we can provide a uniquely wide choice of products to support your analysis, including the key food protein reference materials necessary for allergen characterisation.
InBio has continuously developed new allergen products for 25 years, meaning that Dr Ehrenstorfer customers can now benefit from direct access to their expertise in allergen testing. The InBio ELISA 2.0 kits now available on our website are notable for quantifying specific food allergen proteins of clinical relevance, significantly improving data quality when testing for allergens. InBio’s molecular approach to allergen measurement is to target the clinically relevant allergenic food proteins specifically. This is made possible through manufacturing extensively purified, major allergen proteins that are subsequently used for the development of allergen-specific monoclonal antibodies and ELISAs. Monoclonal antibodies and the analytes they detect can be standardised and used for international harmonisation of allergen measurements - offering users confidence in both the results and their relevancy.
Optimised for ease of operation and designed for inter-lab use with limited variability, InBio ELISA 2.0 kits are a simple to operate detection method suitable for both small and large laboratories. What’s more, they give results in just two hours, and feature pre-coated plates with validated reagents and increased assay sensitivity.
Please click here to see our full range of allergen testing products – which also includes reference materials from the LGC-hosted UK National Measurement Laboratory, Food Allergens Laboratory, the EU Joint Research Centre and Canada’s Conseil National de Recherches. Or get in touch today to find out how we can assist you, whatever your laboratory’s needs.
