NYU study offers new insights into kinase cancer drug resistance
Researchers from New York University (NYU) have shed new light on how cancers can come back stronger after treatment with kinase-blocking drugs.
The findings could have important implications for how clinicians treat patients in future, as well as for the development of new cancer therapies.
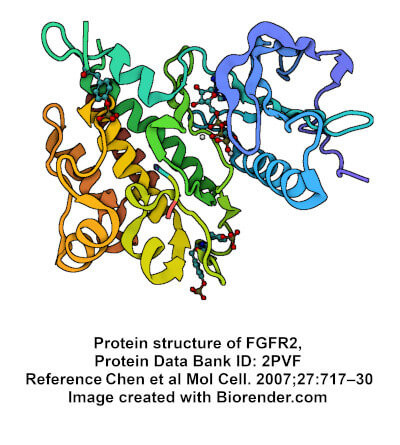
The NYU group used a multi-investigational approach to better understand the mechanism behind drug resistant ‘gatekeeper mutations’ located at the hinge region between the N- and C-lobes of the receptor, near the hydrophobic pocket.
Since kinase inhibitor drugs bind to this pocket to block the binding of ATP, inhibit activation of the enzyme and reduce downstream phosphorylation necessary for cancer signalling and growth, mutations to a kinase’s gatekeeper residue can inhibit a drug’s access - reducing its efficiency, and ultimately leading to resistance.
The gatekeeper residue is most frequently a threonine or valine residue, which usually becomes mutated to a larger hydrophobic residue such as isoleucine, methionine, leucine, and phenylalanine, whose bulkier side chains block access of the inhibitor to the pocket.
Given that almost 40 FDA-approved cancer drugs are kinase inhibitors, this process has serious implications for cancer patients - many of whom suffer aggressive and difficult-to-treat recurrences as a result.
By studying mutations in fibroblast growth factor receptors, or FGFRs – a family of kinases whose mutations frequently cause cancers – the NYU group was able to demonstrate that gatekeeper mutations do not just block access to receptor tyrosine kinase hydrophobic pockets, but may also make the kinases more active.
“When a kinase is switched into the active state, it can lead to processes like cells dividing, a hallmark of cancer,” said the study's first author Alida Besch.
“This increased activity is why we hypothesize that cancers come back even stronger, but exactly how gatekeeper mutations increase kinase activity is not well understood.”
The researchers employed a combination of kinase assays, NMR spectroscopy, bioinformatic analyses and molecular dynamics simulations to study the in vitro activity of V564I and V564E gatekeeper mutations.
Previous studies had suggested that such mutations triggered the active state by strengthening and stabilizing the ‘hydrophobic spine’ - a network of residues connecting different parts of the kinase.
However, the New York investigations suggested that the mechanism worked in a different manner – by destabilising the kinase’s inactive state, thus weakening the hydrophobic spine, and allowing the kinase to shift to the active form.
“We found that these mutations destabilize the autoinhibited conformation of the kinase by weakening the hydrophobic spine and modulating the conformation of the conserved DFG motif,” the NYU group wrote.
“(This led ) to the conclusion that gatekeeper mutations increase in the population of the active state.”
The study’s co-senior author, Yingkai Zhang, said the discovery that gatekeeper mutations destabilised the kinase’s inactive state was “important, because we generally want receptor tyrosine kinases to be held in the inactive state.
“Switching into the active state would usually be dictated by external signals like hormones, not the kinase itself.
“But if gatekeeper mutations are destabilizing the kinase and shifting it into its active form, this could explain why some cancers come back stronger.”
Zhang’s colleague and co-senior author Nate Traaseth said the discovery might also assist doctors treating cancer patients in deciding which drugs – or combinations of drugs – might be most effective.
“If a treatment targets kinases that we know will ultimately mutate, it might be better to use a cocktail treatment right away that will still bind to the kinase, even if the gatekeeper is mutated,” he said.
The NYU group is now considering how the findings might be used to develop new cancer therapeutics – including drugs that could bind more precisely to other locations in the kinase instead of just to the hydrophobic pocket.
“There's not a single kinase drug on the market that only hits one type of kinase, although that is the goal,” Traaseth added.
“Having drugs bind to different spots of the kinase that are more diverse than the hydrophobic pocket is one way to address this challenge.”
|
TRC oncology research chemicals
TRC has more than 40 years’ experience working through some of the most complex synthetic pathways to deliver you high quality research chemicals. We have a uniquely large range, including API, drug derivatives and bioactive molecules. TRC cancer research chemicals include a comprehensive selection of protein kinase inhibitors targeting the FGFR, many other RTKs and downstream effectors, while our world-leading chemists are expert in engineering specific solutions for customers. We also offer an unparalleled collection of ATCC in vitro tools, for cancer research and personalised medicine, including patient derived organoids and immuno-oncology reporter lines, as well as the world’s largest collection of cancer cell lines.
|
